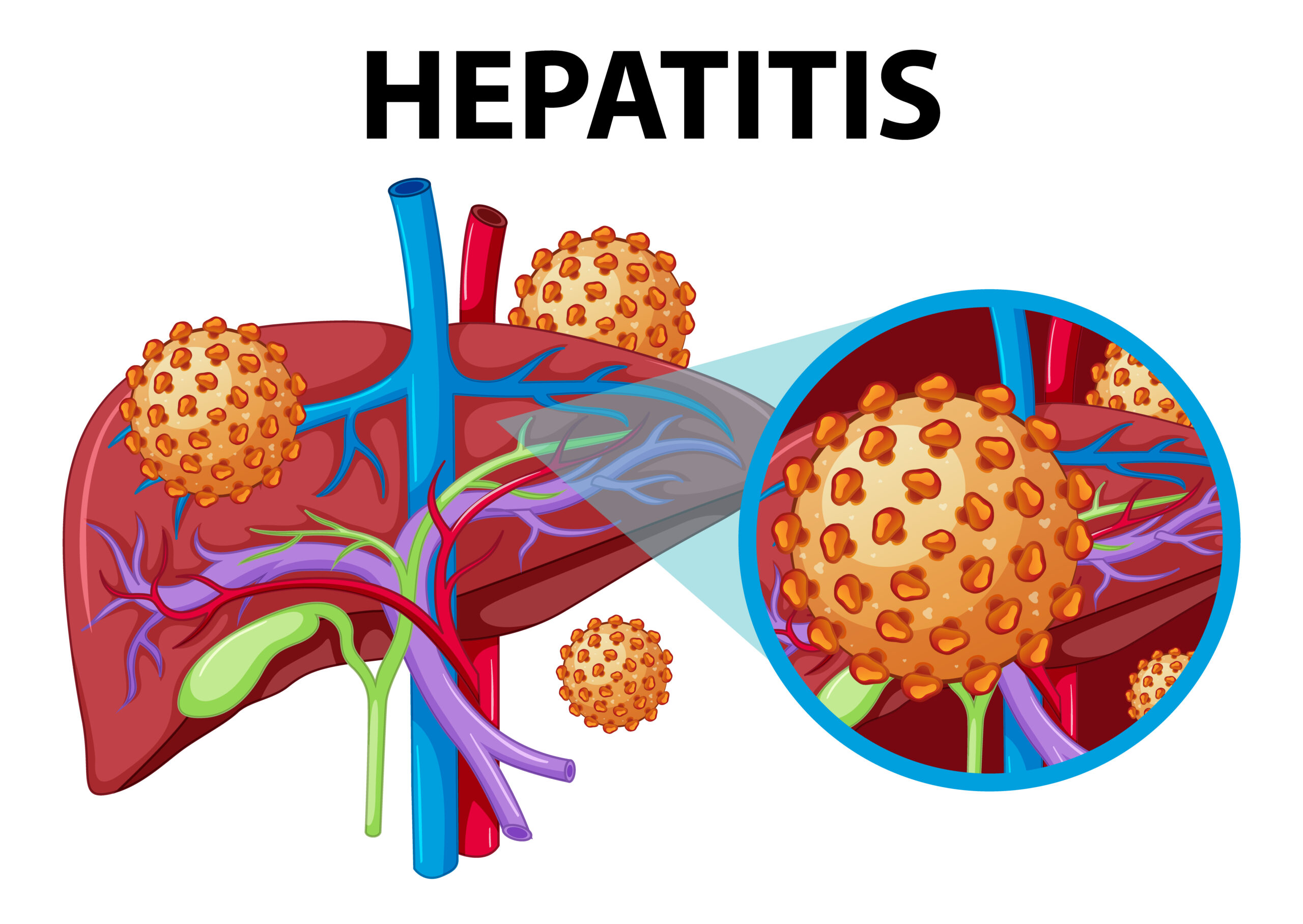
If you are experiencing persistent fatigue, unexplained digestive issues, or subtle changes in your skin, these may be early signs of autoimmune hepatitis symptoms. Autoimmune hepatitis (AIH) is a chronic condition in which your immune system mistakenly attacks healthy liver cells, causing inflammation, liver damage, and potential long-term complications if not managed early. Recognizing the earliest signs of AIH is crucial because timely intervention can slow disease progression and improve overall liver health.
Autoimmune hepatitis symptoms can appear gradually and may vary from person to person. They often include fatigue, poor appetite, joint discomfort, jaundice, and digestive disturbances. In this article, we explore the most common autoimmune hepatitis symptoms, potential causes, diagnosis, medical treatments, functional nutrition approaches, lifestyle strategies, and when to seek professional help. By understanding these symptoms thoroughly, you can take proactive steps toward healing and work with experts like Smriti Kochar to support your liver and immune system naturally.
What Is Autoimmune Hepatitis?
Autoimmune hepatitis is a chronic liver condition in which the immune system attacks liver cells, causing inflammation that can lead to liver scarring or cirrhosis if untreated. It is a relatively rare condition, but early recognition of autoimmune hepatitis symptoms is essential for effective management.
Types of Autoimmune Hepatitis:
- Type 1 AIH is the most common and often associated with other autoimmune disorders such as thyroid disease or celiac disease. It can occur in both teenagers and adults and is more common in females.
- Type 2 AIH is rarer, more severe, and typically develops in children and young adults, predominantly in females.
Who is at risk?
- Women are more susceptible than men, with a ratio of approximately 3 to 4 to 1
- Individuals with a family history of autoimmune diseases, including lupus, thyroiditis, or celiac disease
- Genetic predisposition combined with environmental or viral triggers
Early detection of autoimmune hepatitis symptoms is often challenging because the disease can remain silent for months or even years, making awareness and routine liver function testing critical.
The Most Common Autoimmune Hepatitis Symptoms
Understanding autoimmune hepatitis symptoms is key to recognizing the disease early and preventing long-term complications. Symptoms can be subtle initially and may progress over time.
Early-Stage Symptoms
- Persistent fatigue that does not improve with rest
- Mild abdominal discomfort or tenderness, especially in the upper right quadrant
- Nausea or poor appetite, often accompanied by weight loss
- Joint pain and stiffness
Progressive Symptoms
- Yellowing of the skin and eyes, known as jaundice
- Dark-colored urine and pale or clay-colored stools
- Skin changes, including rashes, vitiligo, or psoriasis-like conditions
- Unexplained bruising or bleeding due to impaired liver function
Advanced Symptoms
- Swelling in the abdomen (ascites) due to fluid buildup
- Swelling in the legs and feet (edema)
- Confusion, memory lapses, or brain fog due to hepatic encephalopathy
- Severe fatigue and weakness interfering with daily activities
Many people with autoimmune hepatitis do not recognize autoimmune hepatitis symptoms initially because they can be mild or nonspecific. Regular medical evaluations and monitoring liver function tests are essential for early detection.
What Causes Autoimmune Hepatitis?
The exact cause of autoimmune hepatitis is not fully understood, but several factors contribute to the development of autoimmune hepatitis symptoms.
- Genetic predisposition and immune system dysregulation increase susceptibility
- Viral infections, such as hepatitis A, B, or C, may trigger immune system activation
- Environmental factors, toxins, and certain medications can provoke liver inflammation
- Chronic inflammation and poor gut health may exacerbate autoimmune activity
Functional medicine emphasizes that addressing these underlying causes, especially inflammation and gut imbalances, can help manage autoimmune hepatitis symptoms alongside conventional treatments.
How Autoimmune Hepatitis Is Diagnosed
Diagnosing autoimmune hepatitis involves a combination of medical history, physical examination, and laboratory testing to confirm autoimmune hepatitis symptoms and assess liver damage.
- Blood tests, including liver function tests (LFTs), antinuclear antibodies (ANA), smooth muscle antibodies (SMA), and liver kidney microsomal antibodies (LKM), to detect liver inflammation and autoimmune markers
- Imaging techniques, such as ultrasound or MRI, to evaluate liver size, texture, and rule out other conditions
- Liver biopsy to confirm the diagnosis and determine the degree of fibrosis or liver damage
- Differential diagnosis to exclude other liver diseases, such as viral hepatitis, fatty liver disease, or drug-induced liver injury
Early diagnosis can improve outcomes, as identifying autoimmune hepatitis symptoms before significant liver damage occurs allows for timely treatment.
Treatment and Medical Management
The primary goal of medical management is to reduce liver inflammation, prevent progression, and maintain long-term liver health.
- Corticosteroids, such as prednisone, are commonly used to reduce immune system activity and inflammation
- Immunosuppressants like azathioprine help maintain remission and prevent flare-ups
- Regular monitoring of liver enzymes and antibody levels ensures treatment effectiveness
- In severe cases, or when medications fail, liver transplantation may be necessary
Medical management combined with early recognition of autoimmune hepatitis symptoms improves prognosis and quality of life.
Functional Medicine and Nutrition Approach
Functional medicine focuses on addressing the root causes of autoimmune hepatitis symptoms rather than only suppressing them. Smriti Kochar emphasizes the importance of gut health, inflammation control, and nutrition in managing autoimmune liver disease.
- Healing the gut and balancing the microbiome can reduce triggers for immune attacks
- Anti-inflammatory diets rich in vegetables, fruits, lean proteins, and healthy fats support liver function
- Elimination diets help identify food sensitivities contributing to autoimmune activity
- Stress reduction, sleep optimization, and mindfulness practices enhance immune regulation
- Functional testing, such as GI-MAP, can uncover gut imbalances contributing to autoimmune hepatitis symptoms
By combining nutrition, lifestyle adjustments, and stress management, many individuals experience reduced inflammation and improved liver health.
Lifestyle Tips to Support Liver and Immune Health
Supporting liver and immune health can improve outcomes and alleviate autoimmune hepatitis symptoms:
- Avoid alcohol, processed foods, and added sugars
- Consume nutrient-dense, anti-inflammatory meals
- Include probiotics, prebiotics, and fiber-rich foods to promote gut health
- Manage stress with meditation, breathing exercises, or yoga
- Maintain regular checkups and lab monitoring to track liver function
These lifestyle interventions work best when combined with medical treatment and functional nutrition guidance.
When to Seek Help
Prompt medical attention is recommended if you notice:
- Persistent fatigue or weakness
- Yellowing of the skin or eyes (jaundice)
- Dark urine or pale stools
- Swelling in the abdomen, legs, or feet
- Worsening digestive issues or unexplained weight loss
- Presence of other autoimmune conditions, such as lupus, thyroid disease, or PCOS
Early consultation with a functional nutritionist or medical specialist can help address autoimmune hepatitis symptoms before significant liver damage occurs.
Real Healing Is Possible with Expert Guidance
If you are experiencing autoimmune hepatitis symptoms, working with Smriti Kochar can help you uncover the root causes, reduce inflammation, and support liver health naturally. Her UltraWellness Program combines functional nutrition, lifestyle interventions, and personalized coaching to restore balance and improve overall well-being.
By addressing both medical and functional aspects, it is possible to alleviate autoimmune hepatitis symptoms, improve energy levels, and support long-term liver function.
Conclusion
Recognizing autoimmune hepatitis symptoms early is critical to preventing liver damage and improving overall health. Symptoms range from fatigue, nausea, and joint pain to jaundice, abdominal swelling, and cognitive disturbances. Early detection combined with medical treatment and functional approaches, such as gut healing, anti-inflammatory nutrition, and lifestyle optimization, can significantly improve outcomes.
Working with a functional nutritionist like Smriti Kochar can help uncover the root causes of inflammation, restore liver and gut health, and reduce autoimmune hepatitis symptoms naturally. True healing begins by addressing the underlying factors inside the body rather than merely treating symptoms.
Read Our Latest Blogs
Autoimmune Encephalitis Symptoms | Autoimmune Disease ICD 10 | Autoimmune Hepatitis Panel | Itchy Skin Autoimmune Disease | Rheumatoid Arthritis Symptoms | Rheumatoid Arthritis ICD 10 | What is Rheumatoid Arthritis | What are the 4 Stages of Rheumatoid Arthritis | Rheumatoid Arthritis Specialists | Difference Between Osteoarthritis and Rheumatoid Arthritis | Is Rheumatoid Arthritis Curable
Frequently Asked Questions
Early signs include fatigue, mild abdominal discomfort, nausea, poor appetite, and joint pain. These early autoimmune hepatitis symptoms are often subtle and can be mistaken for other conditions.
There is no absolute cure, but early intervention and combined medical and functional approaches can manage autoimmune hepatitis symptoms and prevent disease progression.
Women, individuals with other autoimmune disorders, and those with a family history of autoimmune disease are at higher risk. Genetics, environmental factors, and infections also contribute.
Yes. Anti-inflammatory, nutrient-rich diets, elimination diets to identify triggers, and liver-supportive foods can help reduce autoimmune hepatitis symptoms and improve liver function.
Diagnosis involves blood tests (LFTs, ANA, SMA, LKM antibodies), imaging such as ultrasound or MRI, liver biopsy, and ruling out other liver conditions.
Steroids are commonly prescribed to reduce liver inflammation. Depending on severity, immunosuppressants may also be used, and functional interventions can support symptom management.
If untreated, AIH can progress to cirrhosis and liver failure. Early recognition of autoimmune hepatitis symptoms and medical management can prevent severe complications.
Regular monitoring every three to six months is typical, but schedules may vary based on disease severity and response to treatment.